|
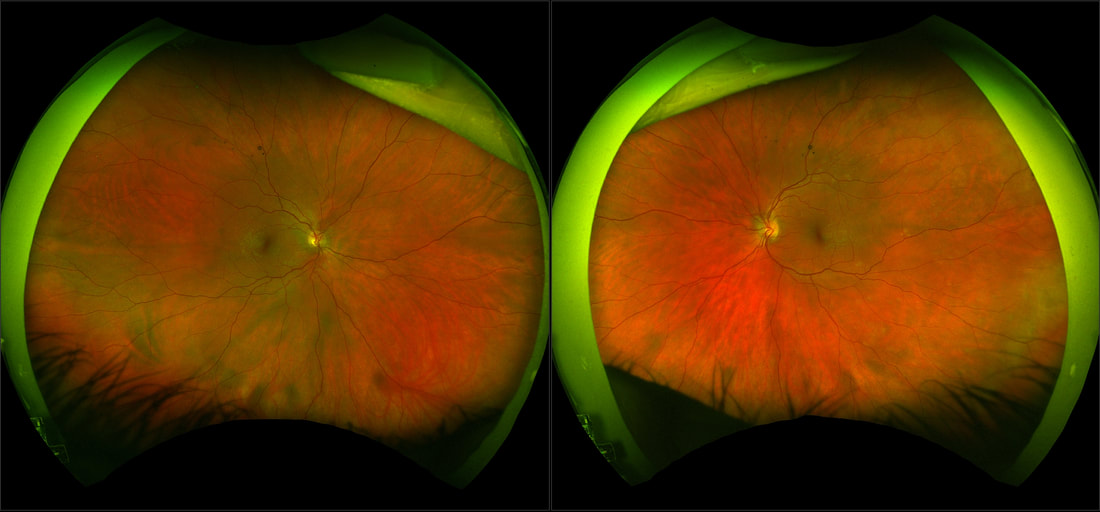
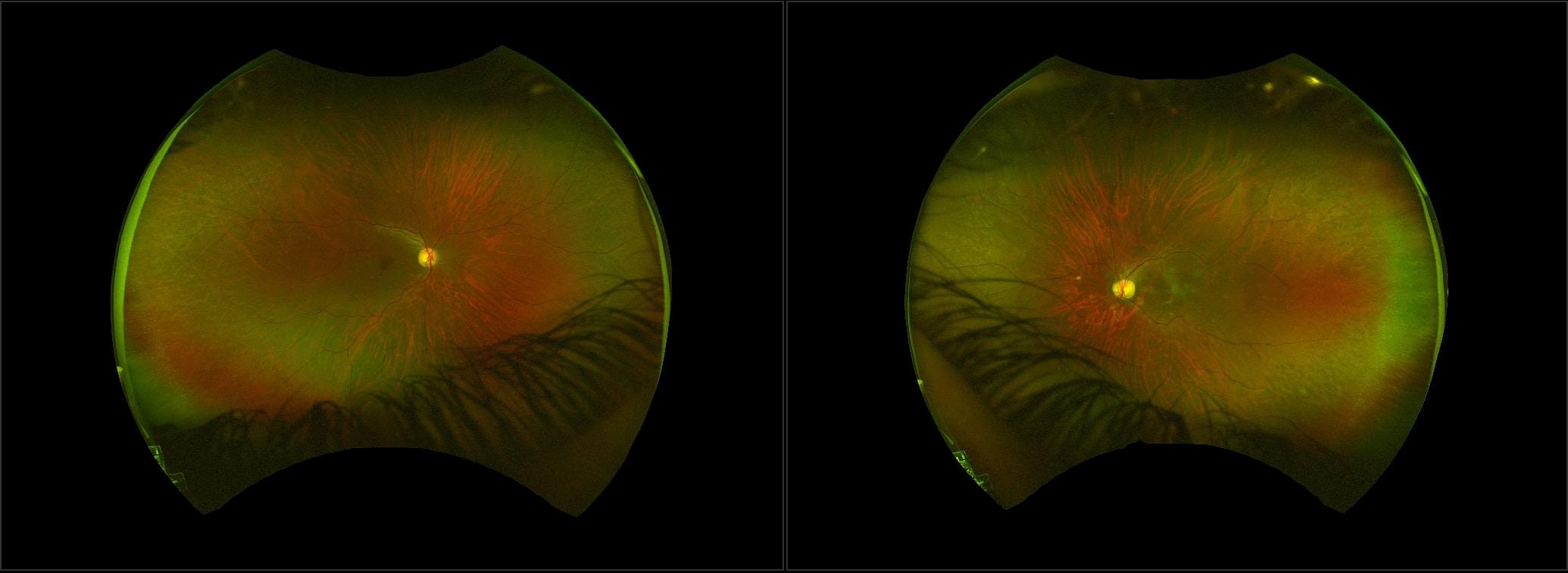
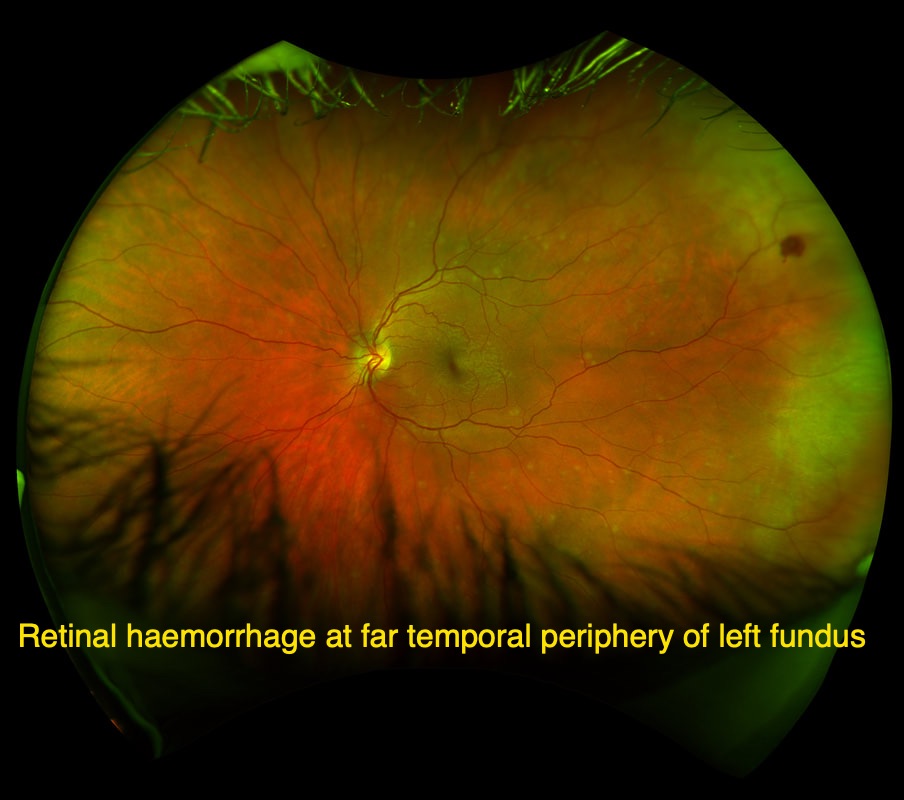
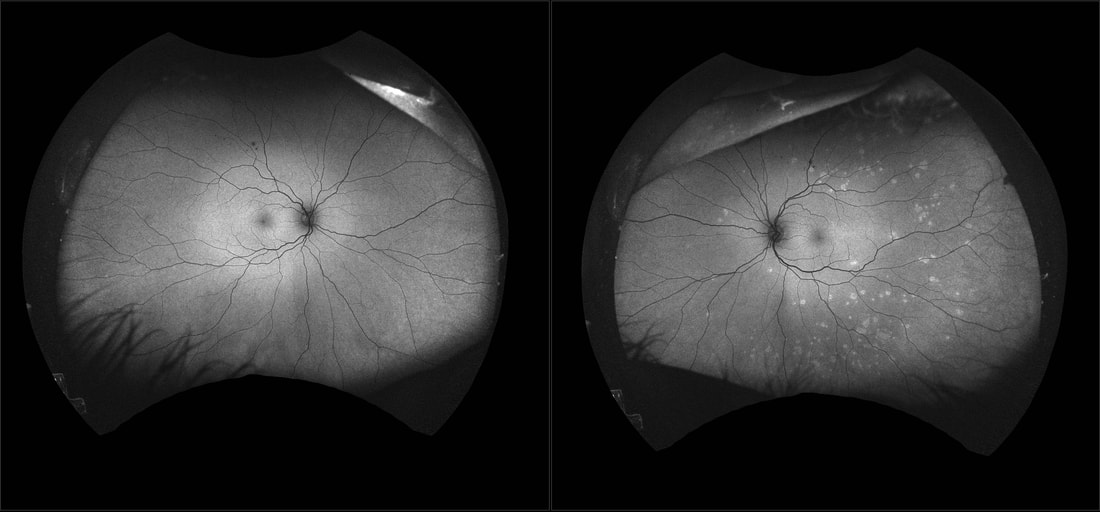
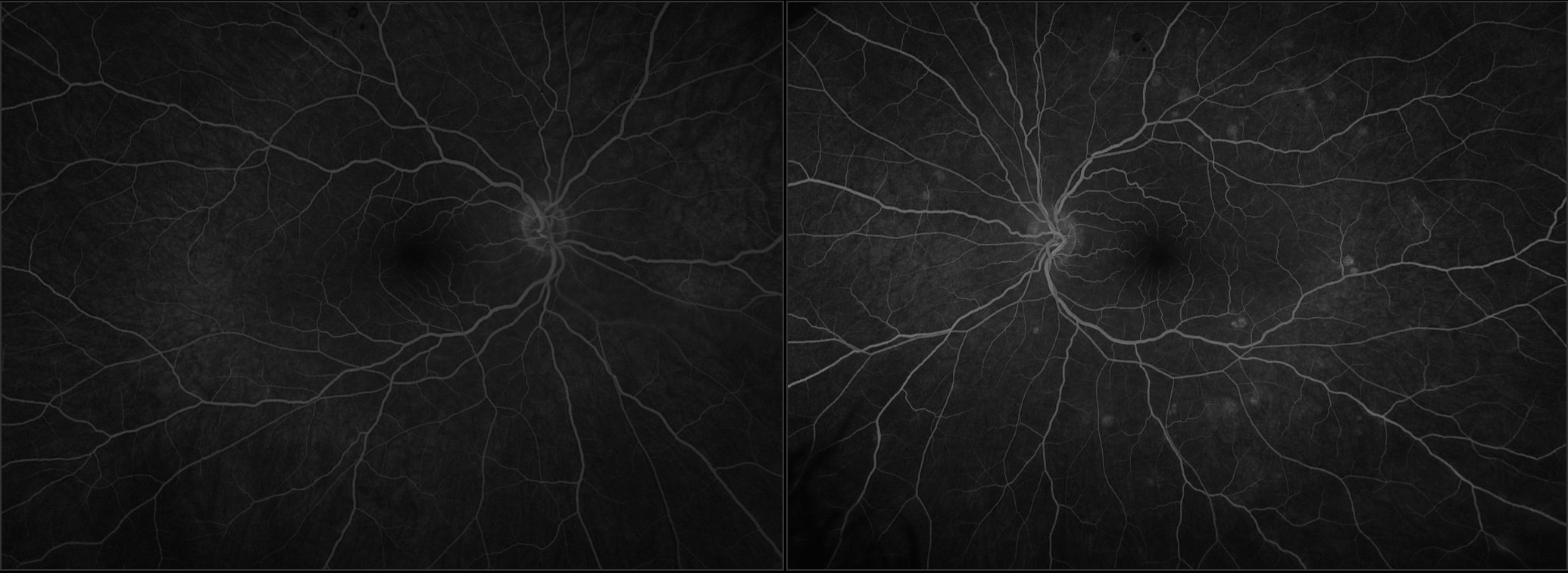
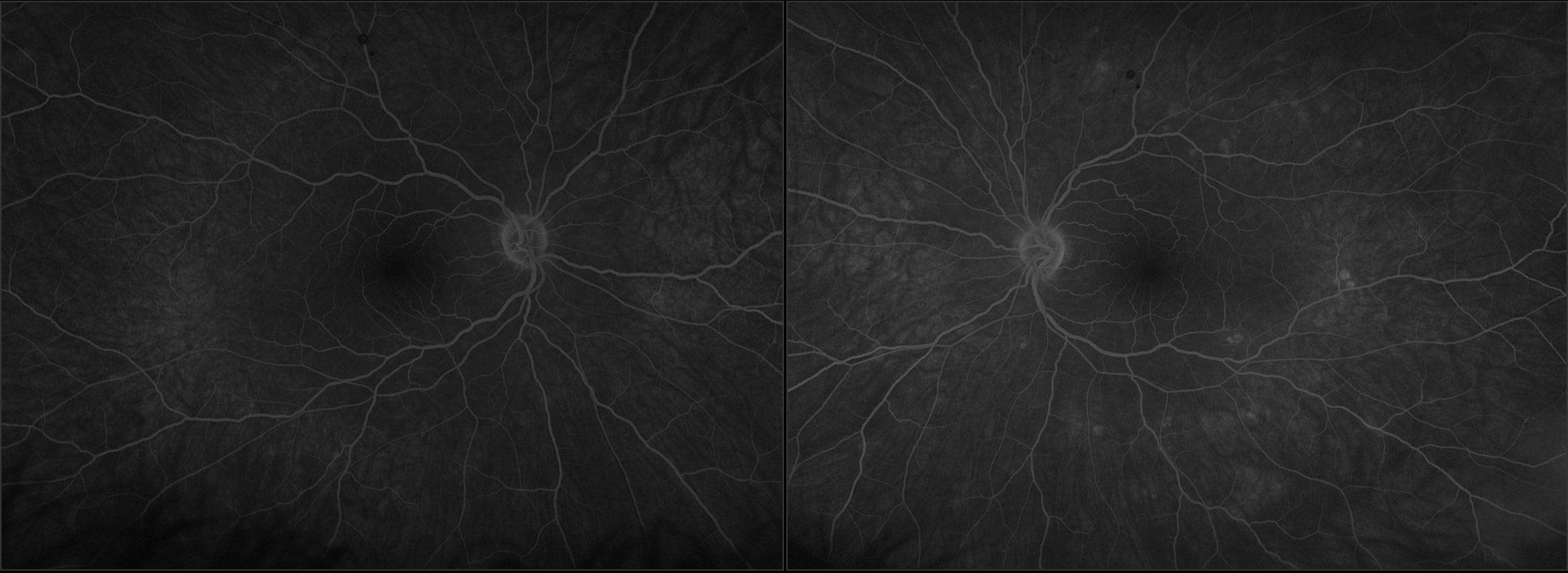
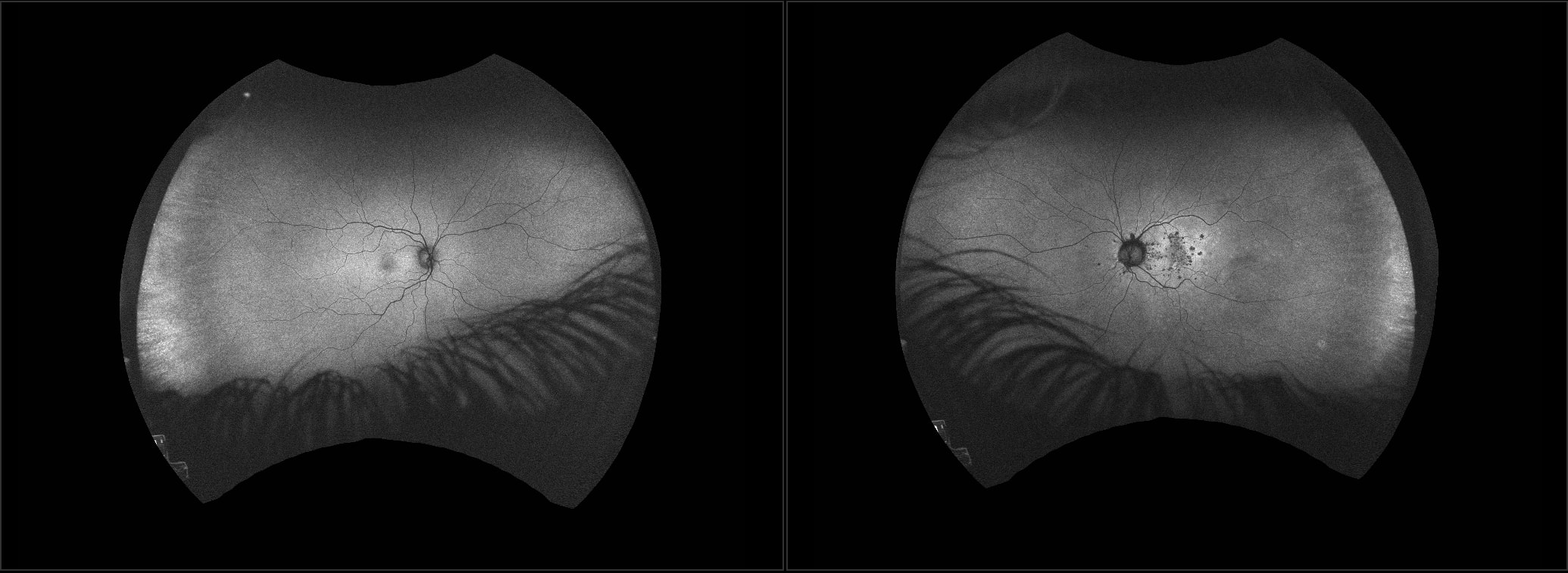
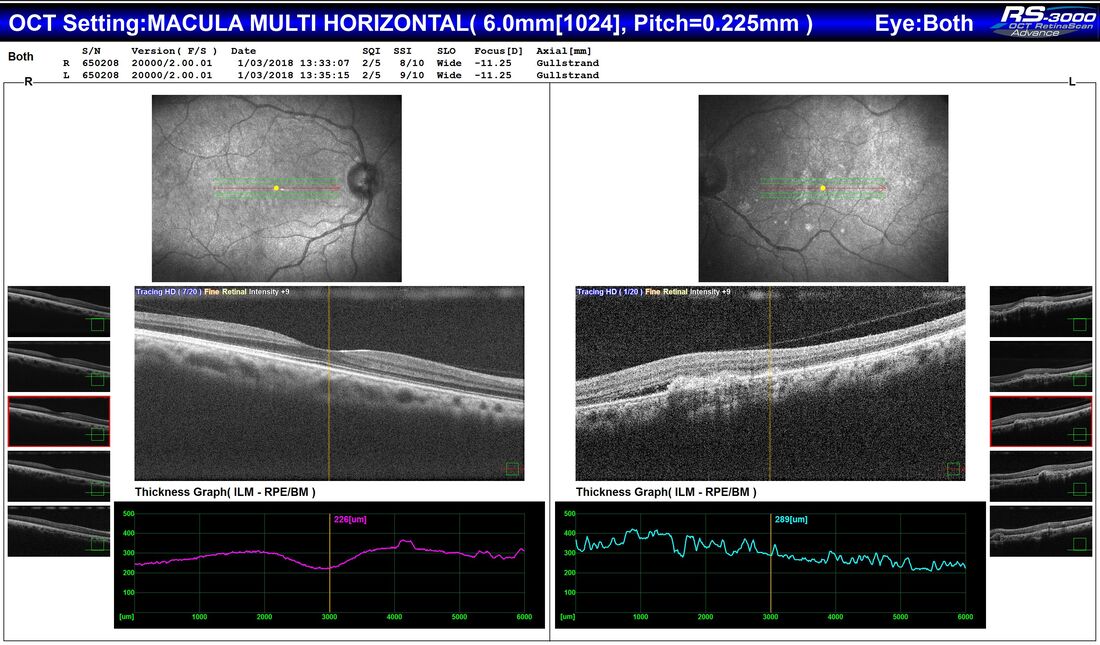
I report two interesting cases referred to South West Eye Surgery CASE 1: A 38 year old woman was referred by her Optometrist with symptoms of flashes and floaters in her left eye over the previous 10 days. There was no reported reduction in vision and her Optometrist observed a small temporal retinal haemorrhage and left choroiditis. She had been well and reported no prior illness. The patient's visual acuity was measured at 6/6 in both eyes. Her fundus examination revealed a small left retinal haemorrhage in the far left temporal periphery and multiple small flat white lesions in the posterior pole outside the macular area in the left eye. Fundus photography showed the lesions to be hyperautofluorescent and revealed further lesions, not easily seen on clinical examination and colour photography, extending out into the mid-periphery and mainly in the left eye. A fluorescein angiogram was performed and this showed early hyper fluorescence of the punctate lesions with late staining. There was also some staining noted in the left disc in the late frames of the angiogram. CASE 2: A 32 year old South American primigravid woman presented to her GP at 23 weeks gestation with a 5 day history of a left central visual field defect, associated with a mild headache occurring at the end of each day. This patient was a moderately severe myope with an -8.00 dioptre correction. She reported that she had suffered from a mild head cold about two weeks before. Visual acuity was 6/9 right and 6/60 left, corrected. The left fundus contained multiple grey/white spots in and around the macula and surrounding the left optic disc. Fundus autofluorescence demonstrated a mix of central hypo-autofluorescent and peripheral hyper-autofluorescent lesions affecting the posterior pole on the left. The Optical Coherence Tomography scan revealed subretinal fluid around multiple dome shaped hyper-reflective lesions in the subretinal space. DIAGNOSIS, TREATMENT AND CLINICAL COURSE: Both patients were diagnosed with Multiple Evanescent White Dot Syndrome (MEWDS) and managed conservatively. At 2 week review, Case 1 reported no more photopsia or floaters and vision remained 6/6 bilaterally. In Case 2, by 2 weeks, vision had improved in the left eye to 6/9 and, by week 4, was back to 6/6 corrected. The central scotoma fully resolved. Multiple Evanescent White Dot Syndrome (MEWDS): MEWDS is one in a group of white dot syndromes. It was first described in 1984 by Jampol and colleagues (1). It is thought to result from inflammation of the retina and choroid of unknown cause. It occurs commonly in otherwise healthy, young, myopic females. Typically, it has an acute presentation in one eye, but bilateral cases do occur rarely. In a third of cases, there can be a preceding viral-like illness. The retinal haemorrhage in Case 1 is a rare associated feature in MEWDS. The syndrome is self-limiting and the prognosis is excellent. Most patients recover full visual acuity and visual field over a period of one to two months. Extremely rarely, chorioretinal scarring and choroidal neovascularisation or progression to AZOOR (acute zonal occult outer retinopathy) can occur (2).
Further reading:
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr Vincent Lee, Archives
April 2020
Categories
All
|
Proudly powered by Weebly


 RSS Feed
RSS Feed