|
In the current CoVid-19 situation, many may be wondering how far we go in protecting ourselves and our staff in our day-to-day work. Some of us remain in operation, seeing urgent cases and this may involve patients with acute problems including red eyes, epiphora, allergies, "conjunctivitis" and other ocular presentations which themselves may be a small part of the spectrum of symptoms experienced by patients with CoVid-19. Or, these or other symptoms, may co-exist in patients who have more mainstream features of the disease (hopefully, these latter patients would have been screened out by procedures detailed in my previous post, and have been referred to the local hospital for further assessment).
In any case, what protective equipment should we be donning to shield ourselves from potential infection?
0 Comments
I share with you some important eyecare-specific information, from the American Academy of Ophthalmology and the Royal Australian and New Zealand College of Ophthalmology, related to the novel coronavirus, referred to as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The highly contagious virus can cause a severe respiratory disease known as Corona Virus Disease - 2019 (COVID-19). (My region-specific advice for South West and Western Victoria are included in red)) Background information on COVID-19: Symptoms can appear as soon as 2 days or as long as 14 days after exposure. The virus is believed to spread primarily via person-to-person through respiratory droplets produced when an infected person coughs or sneezes. It also could be spread if people touch an object or surface with virus present from an infected person, and then touch their mouth, nose or eyes. Viral RNA has also been found in stool samples from infected patients, raising the possibility of transmission through the fecal/oral route. There is a possibility of asymptomatic transmission. A Feb. 21 report in JAMA details a case of an asymptomatic carrier who possibly infected 5 family members despite having normal chest computed tomography (CT) findings. These reports, however, are preliminary. What you need to know
I report two interesting cases referred to South West Eye Surgery CASE 1:
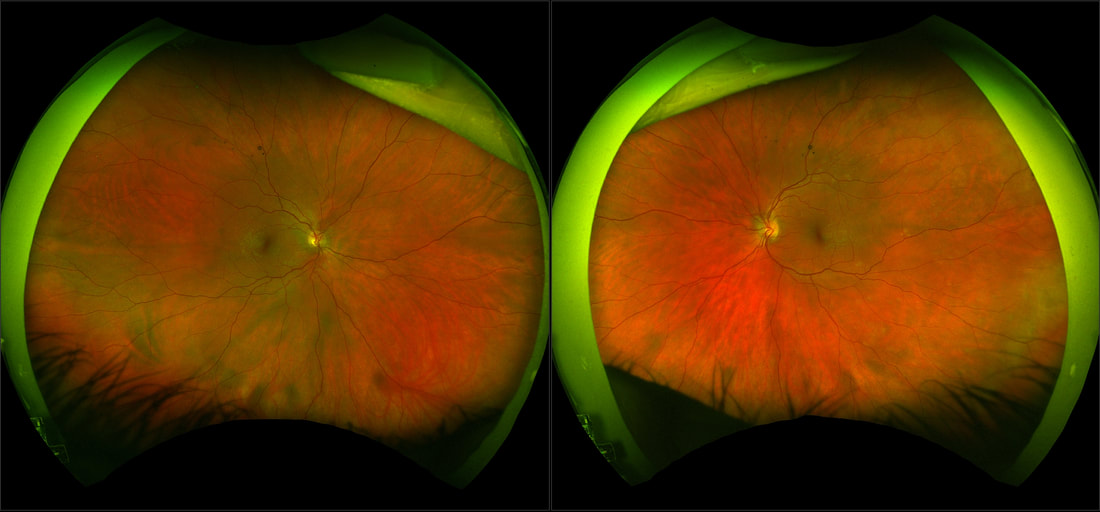
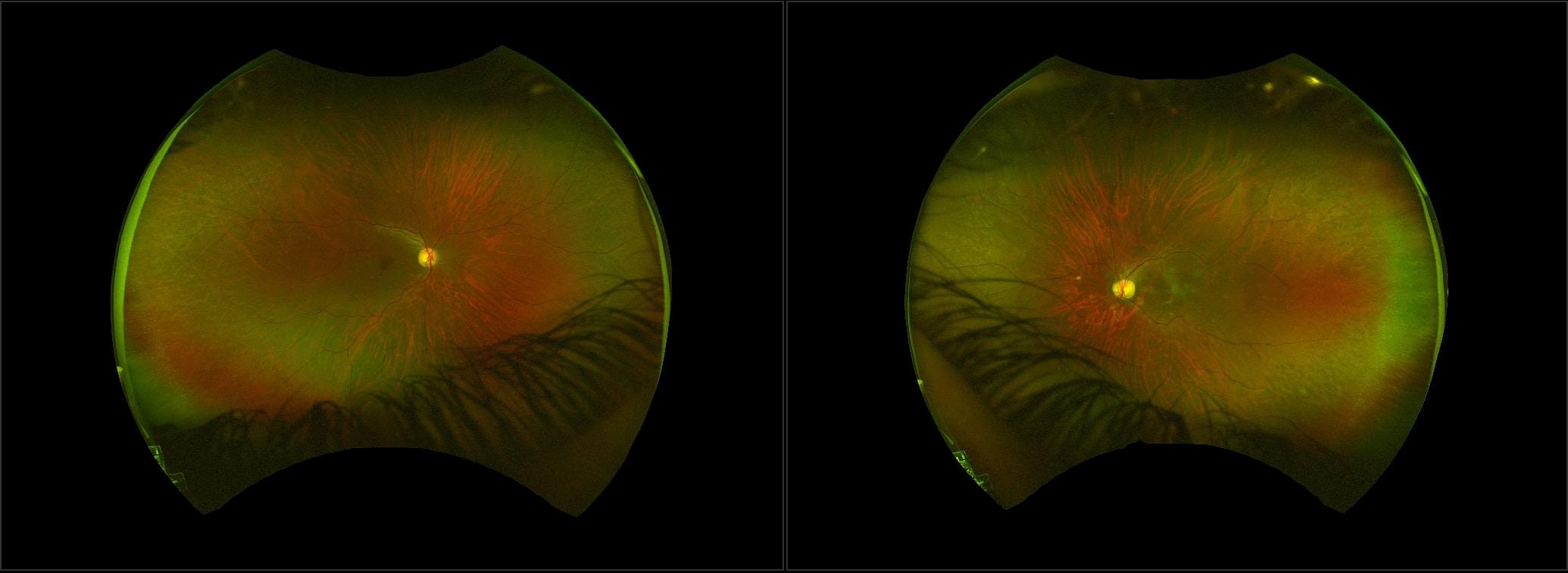
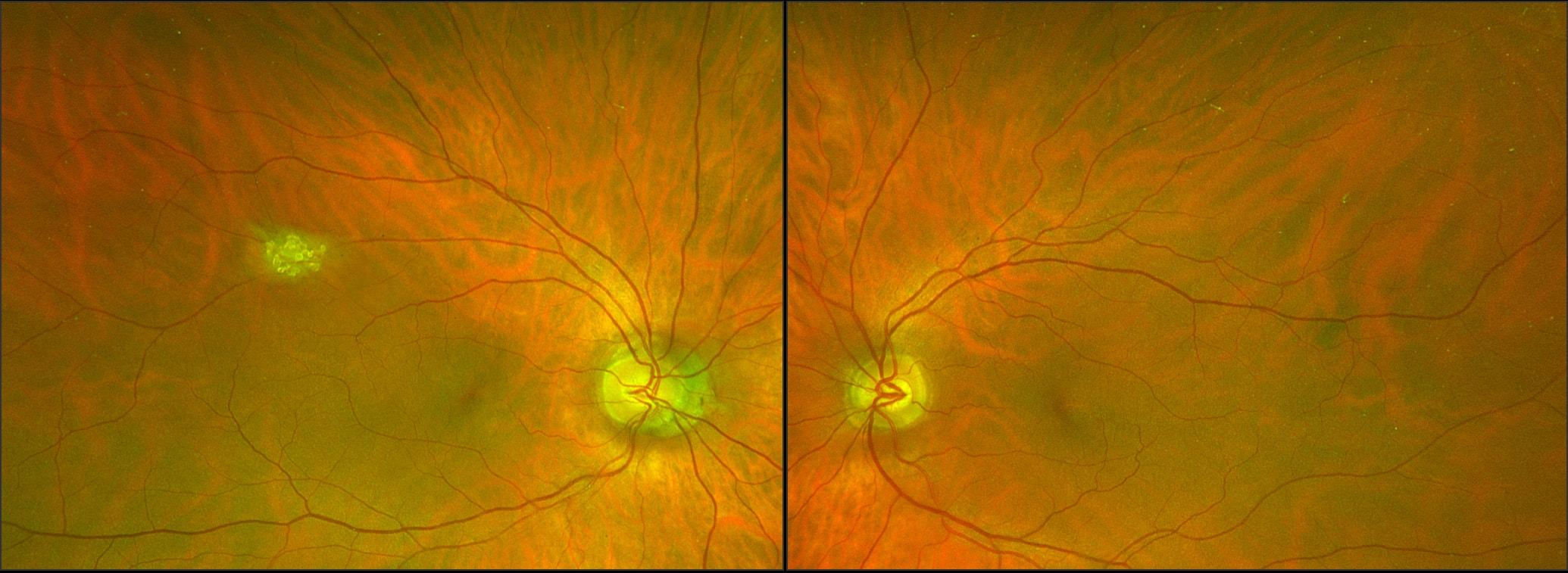
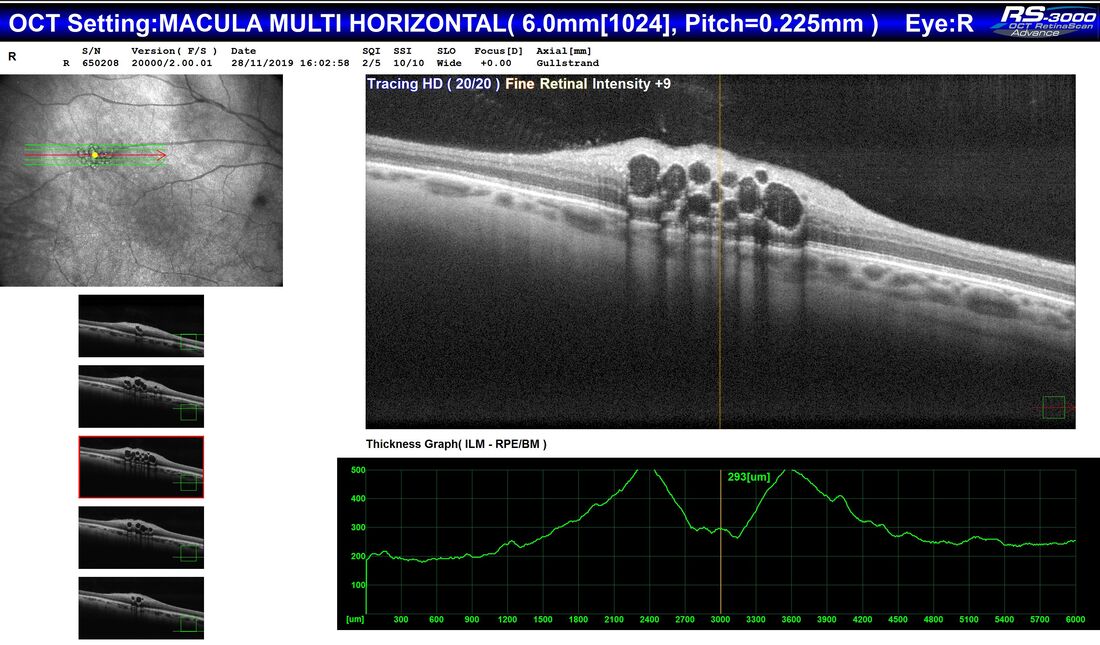
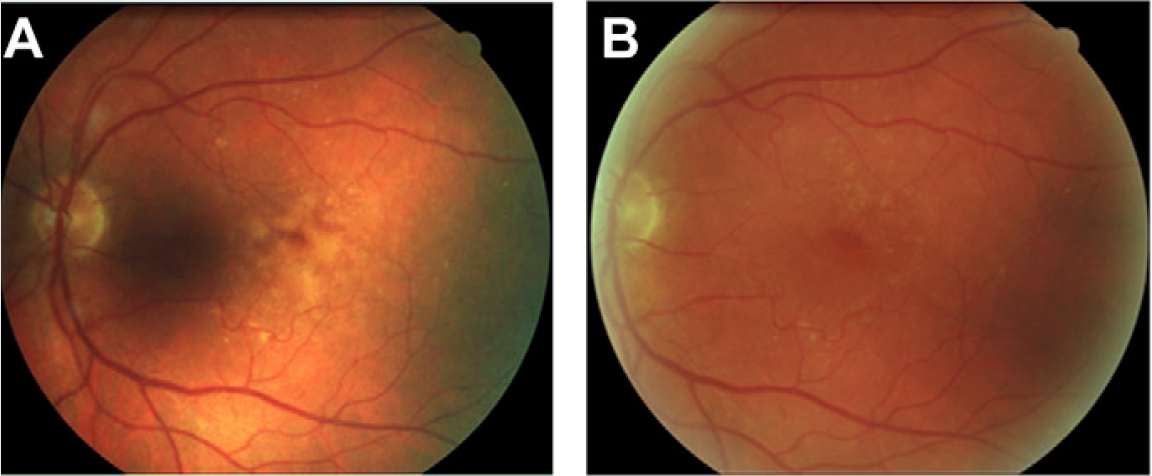
A 38 year old woman was referred by her Optometrist with symptoms of flashes and floaters in her left eye over the previous 10 days. There was no reported reduction in vision and her Optometrist observed a small temporal retinal haemorrhage and left choroiditis. She had been well and reported no prior illness. An otherwise well 65 year old man, during a routine examination for spectacles, was found by an Optometrist to have a lesion in the right fundus that had not been previously documented. There was no relevant past history of any ocular or systemic conditions. The lesion appears raised, white and multinodular, with a scalloped edge and patchy calcification - reminiscent of optic nerve head drusen, but in a peripheral location. On OCT, the lesion appears to have a multi cystic structure, each "cyst" consisting of a hyper reflective edge, casting an optical shadow, with an optically empty centre. This is a typical astrocytic hamartoma or "mulberry lesion" - a benign retinal tumour composed of glial cells (connective tissue cells of the nervous system), predominantly astrocytes. It can occur singly or in multiple locations. It is most often associated with tuberous sclerosis (TS) or Bourneville's Disease, but may also be found rarely in patients with neurofibromatosis. Although the finding may point toward a systemic association, it can also be found incidentally on retinal examination as an idiopathic and spontaneous lesion, as in this case.
Apart from recommending the patient have his retina examined periodically in the future, no treatment was required.
The 51st Annual Congress of the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) was held in Sydney over 5 days in November. Celebrating the 50 year anniversary of RANZCO, the meeting showcased top national and international speakers delivering topics covering current and emerging practices in eye disease diagnostics, technology, surgical and medical treatment, including gene therapy. Highlights included presentations on the Bionic Eye* project at the Centre for Eye Research Australia (CERA) and the evolution of laser treatment in the eye, by Prof John Marshall, inventor of the excimer laser used in refractive eye surgery and of the new sub threshold nanosecond laser, or 2RT, now in use for treatment of dry AMD and diabetic macular swelling.
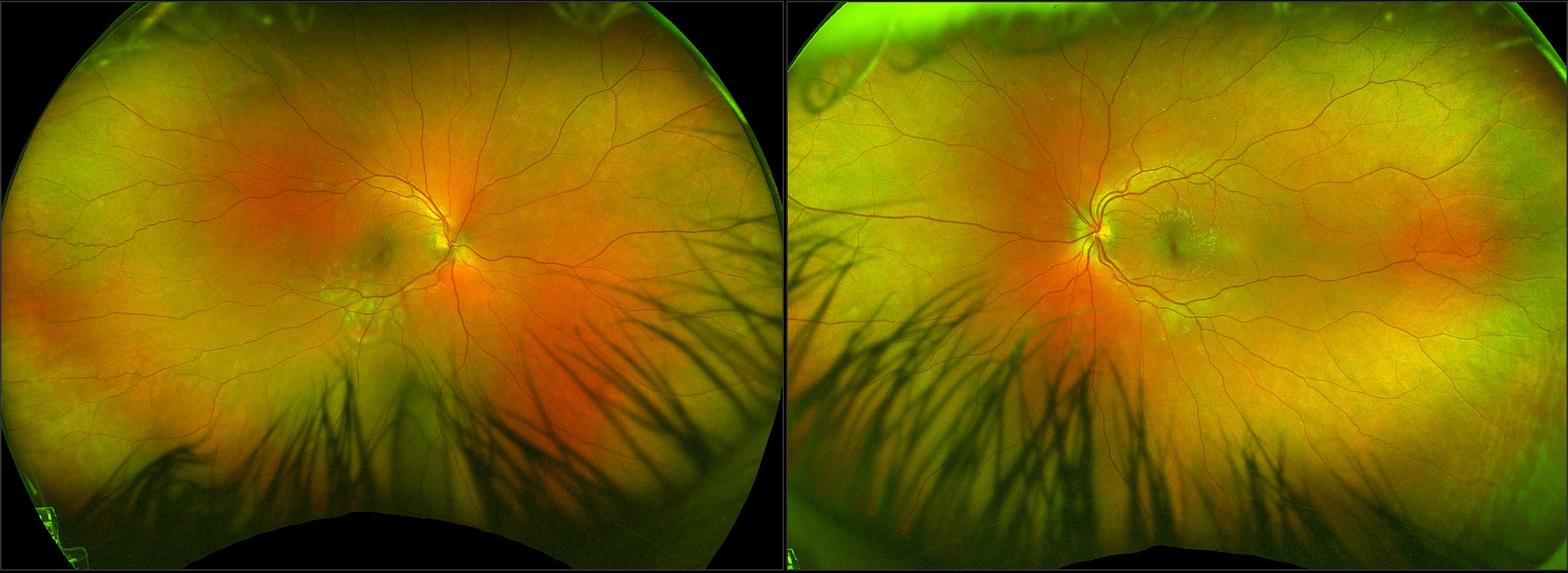
*Associate Professor Penny Allen is delivering the 2019 Gerard Crock Lecture on the Bionic Eye Project on Thursday 21 November in Melbourne. To register for this Free Event click this button: A 21 year old male was referred to South West Eye Surgery by his GP with blurred vision and a central visual field defect (a blurred patch) in his right eye. He had awoken 2 days previously with a headache, fatigue and bloodshot eyes.
On examination, visual acuities were Right 6/12 and Left 6/5. He had bilateral conjunctival hyperaemia (red eyes), but little anterior or posterior uveitis (internal eye inflammation) of note. I attended the 19th Congress of the European Society of Retina Specialists in Paris, early this month.
A gathering of the top minds from Europe, USA, Asia and the rest of the world in the stunning setting of the City of Lights, made for an enlightening meeting . It was a privilege and a pleasure to host the Warrnambool Winter Symposium on the 22nd of August 2019. A gathering of 20 regional optometrists (representing all the Optometry practices in the Southwest and Western Districts of Victoria), clinical staff and industry representatives assembled for a cosy dinner on a cold August evening, at the Lady Bay Hotel Warrnambool, to hear about the latest developments in treatment of Age-related Macular Degeneration (or AMD, as well as Diabetic Macular Oedema and Retinal Vein Occlusions) and Refractive Surgery. The meeting was approved for 2 CPD points by Optometry Australia.
I was invited to present a lecture on the management of Diabetic Retinopathy (DR) at the Lady Bay Conference Centre at the end of July. The meeting was attended by GPs in Warrnambool and surrounding districts, as well as industry representatives. The intent of the DR Insight meeting is to accelerate awareness amongst General Practititioners about DR screening pathways in primary care settings. Welch Allyn and Mylan Pharmaceuticals, as part of the Keep-Sight program https://www.keepsight.org.au/, host multiple educational events across regional Australia. The educational events include a presentation delivered by an Ophthalmologist and an Endocrinologist (Dr Shannon McCarthy, Epworth Geelong) along with hands on experience with the RetinaVue device to increase awareness of DR screening & demonstrate the unique telehealth component of the RetinaVue camera. ICL (Implantable Collamer Lens) vision correction surgery gives patient "High Definition TV" vision8/5/2019
In what is likely to be the first operation of its kind in regional Australia, a 32 year old patient from Hamilton last week received an Implantable Collamer Lens (ICL or Intraocular Contact Lens or Phakic Intraocular Lens) at St John of God Hospital in Warrnambool.
The 20 minute operation was performed by Warrnambool Eye Specialist Dr Vincent Lee and involved inserting a very thin lens into each of the patient's eyes to remove the need for glasses or contact lenses. The patient made a rapid recovery. Immediately after the operation, she was able to see well enough for the first time to walk around safely without thick spectacles or contact lenses. By the next morning, the patient's vision in each eye was excellent, measuring 6/9, without the help of spectacles. On day 2, she reported that her vision was so clear it was like she was "watching a High Definition television". At the 1 week check, her vision was effortlessly 6/6 or 20/20. The Implantable Collamer Lens or ICL is like a contact lens but, rather than sitting in front of the eye on the cornea, it is placed inside the eye and therefore, is permanent and does not have to be removed each night or each week. The patient is a young professional who had required very thick spectacles (-11.00 diopters) for severe myopia or short sight from the age of 6 years. She said that by the time she was in high school, Warrnambool is the first regional city in Australia to receive the revolutionary 2RT laser for the treatment of age-related macular degeneration (AMD) and diabetic CSME (vision-threatening swelling of the macular in diabetes), with the installation of a new laser machine at South West Eye Surgery in Koroit Street. The sub threshold nanosecond laser, known as 2RT - Retinal Rejuvenation Therapy, is the first laser shown to be able to safely reverse the early signs of AMD and slow down progression to the late stages of the disease, which leads to vision loss and the need for eye injections. The 2RT laser is also able to treat diabetic CSME without the associated collateral damage to adjacent retina as seen with laser retinal photocoagulation. In AMD, despite the advent of improved screening tools, which has enabled eye physicians to diagnose the disease in its earlier stages, treatment options have remained limited to the late, wet stage of the disease only. Whilst anti-VEGF injections have proven to be a highly effective treatment option in cases of wet AMD, we haven’t been able to treat the large number of patients diagnosed with the disease in its earlier stages. It is estimated that early-intermediate AMD accounts for 85% of all cases of AMD.
Recently, a multi-centre clinical trial at the Centre for Eye Research Australia (CERA), has demonstrated the efficacy of nanosecond laser in slowing the rate of progression from intermediate AMD to late stage AMD in selected patients and therefore reducing the risk of needing life-long eye injections. A major new study has shown that SLT, a non invasive, pain-free laser that has been in use for many years, is better at controlling pressure in patients with open angle glaucoma than conventional eye drops.
Dr Gus Gazzard and colleagues at the world famous Moorfields Eye Hospital in London, UK reported the results of the LiGHT Study, which compared SLT to glaucoma eye drops as first-line therapy in a multi centre randomised controlled trial, in The Lancet journal. 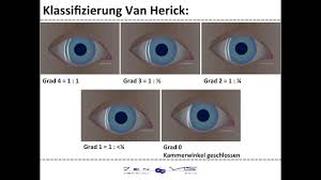 While simple to perform and generally fairly accurate, a recent study has shown that the Van Herick technique for estimating anterior chamber angle depth can be unreliable in some circumstances. This applies to males and myopes (people with short sight). The other risk factors are when this technique is performed on individuals of Asian and black race. Click the button to read an abstract of the study: As such, it is recommended that when examining people in this demographic, a more reliable test is gonioscopy, especially when performed in a dark room. 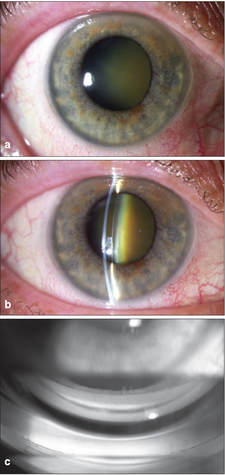 One system of grading the anterior chamber angle depth is the Shaffer grading system, as depicted below: 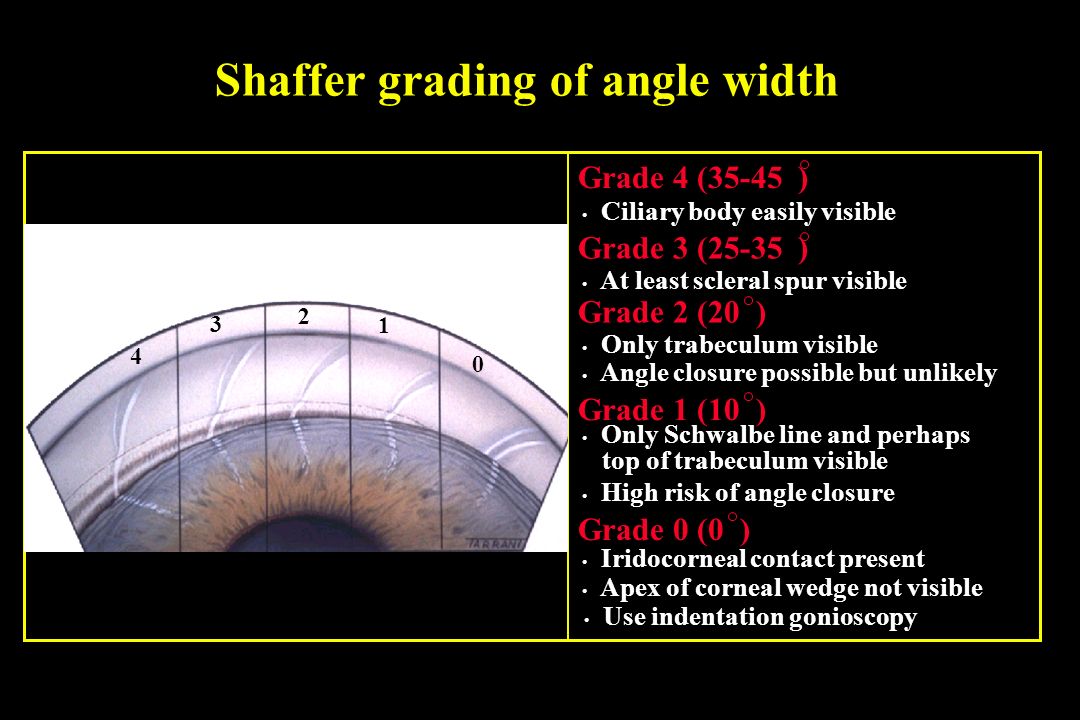  Zovirax® (aciclovir) 3% eye ointment will be discontinued and deleted from the market in February 2019 after GSK ceased manufacturing in the 3rd quarter of 2018. When existing supplies of Zovirax® (aciclovir) 3% eye ointment are exhausted the following options may be considered:
*Please note that I have made arrangements for the Pharmacy Departments at St John of God Hospital and South West Health Care to ensure they carry stocks of AciVision® for prescribers in Warrnambool. Patients will simply need to present their prescriptions to access the drug. I will be speaking to Pharmacy Departments in Colac and Hamilton soon to ensure this brand of aciclovir is made available. If prescribers have difficulty accessing this drug for their patients, please contact me directly - Dr Vincent Lee. 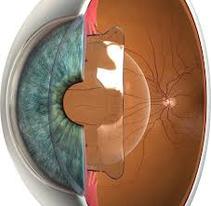 For short sighted people who want a permanent solution to get rid of their spectacles, LASIK has been a go-to choice for a long time. However, many are not suitable for LASIK - their level of shortsightedness may be too high or their corneas too thin, or too irregular, or too dry. There are also a proportion of patients in whom shortsightedness returns after their LASIK procedure. Furthermore - a process termed regression, LASIK is tissue-destructive - a thin layer of cornea is removed in reshaping its surface and it cannot be repeated more than once, if an incorrect result is obtained at the first attempt. Finally, when cataracts eventually develop, post-LASIK patients, will find that their options are limited when it comes to whether they can have premium Intra Ocular Lenses (IOLs) to enable them to remain spectacle free after cataract surgery. This is due to the higher order aberrations created by the laser procedure (from unpreventable tiny movements of the eye during the laser re-shaping process). So a procedure that frees you from glasses in your younger years may actually reduce your chances of being spectacle free in the second half of your life. 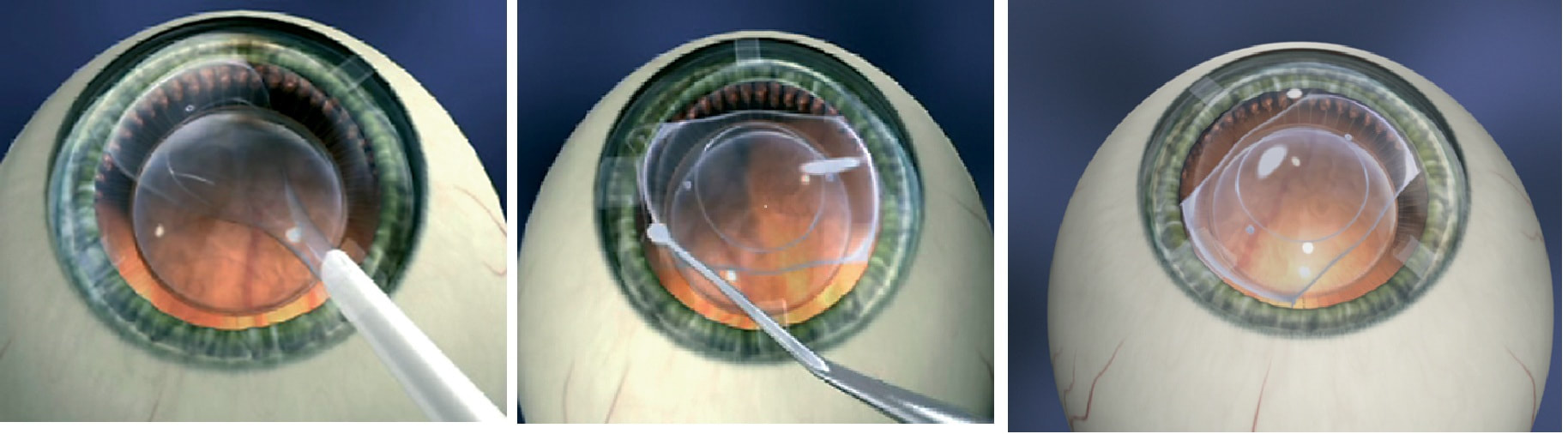 However, shortsighted people can choose another procedure, known as ICL (or Implantable Collamer Lens/ Intraocular Contact Lens or Phakic IOL). The ICL procedure does not have any of the above disadvantages of LASIK and has a number of additional benefits that may give it an advantage over LASIK, as explained yesterday at a meeting of the American Academy of Ophthalmology, in Chicago. Click the button below to access the link to the AAO webpage: Click the button below to learn more about the ICL
Today, 2 of our patients became the first to receive a Hydrus Microstent implant in Victoria. The Hydrus is the latest MIGS device to be approved for use in Australia by the TGA (Therapeutic Goods Administration).
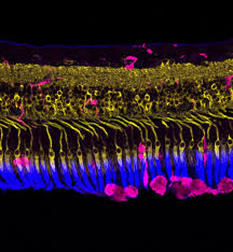
MIGS or, Minimally Invasive Glaucoma Surgery, is a new class of surgery which is considerably less invasive than traditional glaucoma surgery. The use of microstents and other MIGS procedures has greatly reduced the burden of eye drops in glaucoma sufferers with nearly all patients experiencing a reduction in the need for glaucoma eye drops following this type of surgery and many patients not requiring any drops at all. The surgery was performed by Dr Vincent Lee at St John of God Health Care in Warrnambool. A highlight of the EURETINA Congress held in Vienna in September was the announcement, for the first time, of the results of a study which showed that a new laser treatment - known as Retinal Rejuvenation Therapy or 2RT - reverses the ageing changes in Macular Degeneration (AMD) and leads to a substantial reduction in advancement to the late stages of AMD, including Wet AMD.
Up until this time, there has been no treatment for Dry AMD and the worry for many with this disease has been that there was no preventive therapy that could reduce their chances of progressing to the late stages of Wet AMD. It now appears likely that there will soon be a laser that, simply and painlessly applied to the eye in the clinic over a few minutes, could prevent the late stages of AMD and the risk of requiring monthly eye injections for life! It is very pleasing that the study was conducted in our Victorian capital city of Melbourne, at the Royal Victorian Eye and Ear Hospital, and that the new laser is built just across our state border, in Adelaide! It was a privilege to attend the EURETINA Congress, a meeting of the European Society of Retina Specialists, held in Vienna in September. Apart from the simply awesome city which was the venue of the meeting, it was gratifying to learn that much of the latest technology available to the world, in terms of the diagnosis and treatment of retinal and macular diseases, is also currently available right here in the south west of Victoria.
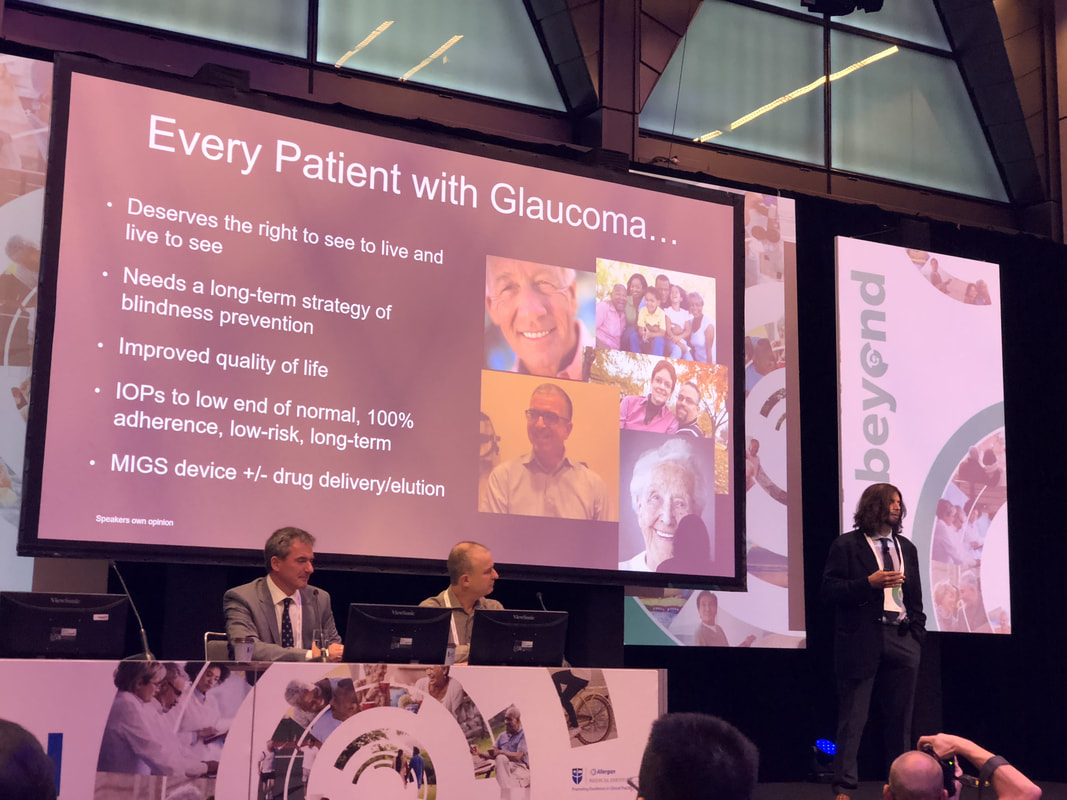
Nevertheless, there was also much to discover in relation to new technology and treatment modalities that are just on the horizon. For example, I was very excited to learn that a number of longer acting drugs and a slow release device are about to be introduced, which will mean that patients, who need regular eye injections for macular disease will soon see benefits in reduced frequency of injections and a longer interval between injections of up to 6 months!  Dr Vincent Lee was an invited speaker at a Bayer sponsored event - "The Health Challenges of an Ageing Population" held at the Quorum, Warrnambool on 7 August 2018. The meeting was attended by General Practitioners, Pharmacists and Nurses. Dr Lee spoke about the skyrocketing prevalence of diabetes and its impact on the health of the population, not just the elderly, but also the young, due to Type 1 and Type 2 Diabetes. Diabetic Retinopathy (DR) and Diabetic Macular Oedema (DMO) are the two main eye complications of the disease which can potentially lead to moderate to severe loss of vision if undetected and untreated The Allergan Beyond conference was held in Sydney on the 21-22 July 2018. An eminent group of world leaders in glaucoma was convened to present the latest information on MIGS, in particular the Xen Gel Stent. The XEN® Gel Stent is a surgical implant consisting of a 6mm long gelatin stent designed to lower high eye pressure in open-angle glaucoma patients where previous surgical treatment has failed and/or medications alone were insufficient (also known as refractory glaucoma). Dr Ike Ahmed from Toronto Canada, widely regarded as a 'guru' of MIGS, was present to pass on some invaluable tips on the use of the Xen stent and his views on the use of this and other MIGS devices.
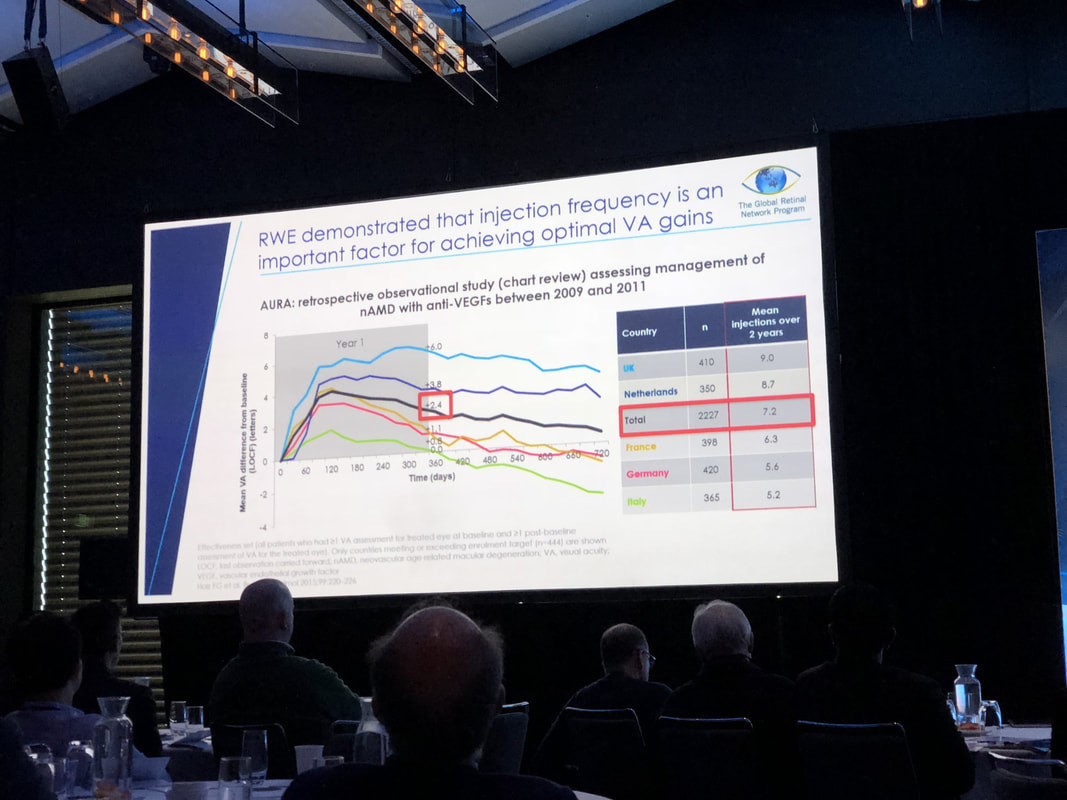 Dr Lee attended the Global Retinal Network Program held on the weekend of 23-24 June 2018 in Sydney. Guest presenters included:
Important updates on the treatment of retinal disease were presented by an international group of experts. For more on this meeting as reported in mivision: Held on the 26-27 May 2018, The Australian and New Zealand Society of Retinal Specialists convened for their annual Retina Symposium in Melbourne. Attended by retinal specialists from Australia, New Zealand and beyond, the meeting was a great opportunity to catch up with developments in the field. MIGS arrives in Western Victoria
There is finally some relief in sight for glaucoma sufferers in Western Victoria with the arrival of Minimally Invasive Glaucoma Surgery (MIGS). Dr Vincent Lee recently delivered a lecture on ‘MIGS Treatment Algorithms’ to a group of 15 Optometrists from the region. The lecture, on 20 March 2018, was organized through Optometry Victoria Director, Mr Jayson Ward of Warrnambool and Portland Eye Care, and held at the Lady Bay Resort in Warrnambool. Attending Optometrists received 3 CPD points, as approved by Optometry Victoria.  The iStent Inject is expected to help glaucoma sufferers by reducing their dependence of eye drops and, in some cases, completely eliminate the need for them. This is the first, widely available MIGS (Minimally Invasive Glaucoma Surgery) device in Australia and was formally approved by the TGA (Therapeutic Goods Administration) Australia, earlier this year, in 2016.  At the invitation of Glaukos Australia, Dr Vincent Lee presented a lecture to Optometrists, GPs and other specialists, at Warrnambool's Lady Bay Resort, on the advent of MIGS and the iStent Inject.  Dr Lee delivered a presentation on Corneal Foreign Body Removal to a group of 14 Optometrists from the Western District of Victoria on November 2015. The Workshop was organised by Optometry Australia and held at the Lady Bay Resort, Warrnambool. Patients are now reimbursed by Medicare for having this procedure performed by Optometrists. This represents formal recognition of the excellent work that had been done by many, but that had not been reimbursed, up till this time. Dr Lee's lecture focussed not just on the finer points regarding the techniques used in FB removal, but also on the importance of recognising other conditions that can mimic corneal foreign bodies. He presented a systematic clinical approach to managing patients presenting with foreign body symptoms that would allow Optometrists to eliminate other potentially sight threatening conditions and proceeded to describe best-practice methods of foreign body removal and complete after care. For more information on the event, click the link below to access the Optometry Australia webpage: |
AuthorDr Vincent Lee, Archives
April 2020
Categories
All
|
Proudly powered by Weebly






 RSS Feed
RSS Feed